AWARDEES: Dr. Katalin Karikó, Dr. Drew Weissman
FEDERAL FUNDING AGENCIES: National Institutes of Health
Katalin Karikó. Photo credit: Bela Francia
In 1997, the photocopier at the University of Pennsylvania (Penn) Department of Medicine was a hot commodity. Unlike today, when online scientific articles are available at our fingertips, back then articles were only accessible in physical scientific journals. If a researcher wanted to read a study, they would have to make the trek to the department office to scan and print a separate hard copy. At Penn, new faculty member Drew Weissman found himself jockeying for space with one researcher in particular, a scientist named Katalin Karikó.
Drew Weissman. Photo by family friend
Today, over two decades and many research hours later, Weissman likens his research partnership with Karikó to an old Reese’s peanut butter cup commercial — “You got chocolate in my peanut butter!” The two complement each other. Karikó, now a Senior Vice President at the pharmaceutical company BioNTech, is exuberant; she lights up when she describes her research. Weissman, who still leads a lab as the Roberts Family Professor of Vaccine Research at the Penn School of Medicine, presents a more serious exterior. Karikó says he isn’t into small talk, joking that he’s limited to a certain number of words per day.
Often, while waiting for the photocopier to spit out the desired pages — or fixing a dreaded paper jam — Karikó and Weissman dove into discussing research. Weissman explained that he wanted to make a vaccine for HIV. Karikó, a self-described “RNA-pusher” at the time, told him she could make any mRNA he wanted to test. Neither knew that the partnership originating from these conversations would go on to pull a research area from the edge of obscurity and transform it into a source for lifesaving vaccines and therapies.
The Molecule that Started it All
Oddly enough, RNA — the hero of this story — is a molecule that plays a crucial part in a cellular process that bears striking resemblance to photocopying. RNA, or ribonucleic acid, is a molecule closely related to DNA, the molecule that encodes all genetic instructions for living things, including recipes for proteins integral to a functioning body. However, DNA and its encoded instructions are trapped within a holding container, the nucleus, while proteins are manufactured outside the nucleus in a completely different part of the cell. That’s where messenger RNA (mRNA) comes in. mRNA is a special type of RNA that makes a copy of DNA’s protein-making instructions and delivers them to the factory of the cell, which uses the copied instructions to produce proteins.
The Research Begins
Karikó began her research career studying RNA in Hungary, where she completed her PhD in Biochemistry. She studied a molecule known as “2-5A,” which jump starts a process that interferes with viral replication. She continued her research in Hungary until her postdoctoral fellowship ran out of money, and she sought a new position in the United States.
The move was anything but easy — at the time, the Hungarian government allowed citizens to take the equivalent of just $100 out of the country, not enough to start a new life somewhere else. Karikó and her husband sold their car on the black market and sewed the proceeds into their two-year-old daughter Susan’s teddy bear, which they carried to the U.S.
Katalin Karikó in 1985
Several years later, Karikó began working at Penn as a research assistant-professor with Dr. Elliot Barnathan, a cardiologist, focusing on mRNA. At the time, RNA was not an attractive research area — the molecule is notoriously tricky to work with because it quickly disintegrates in both laboratories and cells. The researchers’ grant proposals were repeatedly rejected because others didn’t see their work as worthwhile. Yet Barnathan and Karikó persisted, and eventually got their breakthrough. By delivering mRNA into cells, they could induce the cells to make a protein that the cells did not typically manufacture. “I felt like a god,” remembers Karikó. However, the celebration was short lived. Barnathan left Penn for a job at a biotech firm in 1997, leaving Karikó with insufficient grant support to stay at the university, unless she could secure another lab to work in.
Undeterred, Karikó found places to continue her research; she notes her gratitude for her colleague David Langer, a neurosurgeon who convinced his department’s chairman to provide lab space and a salary for her. Karikó found refuge — and joy — in the lab. It would be years until she saw large returns on her work, but her next research partner would catalyze the process.
Meanwhile, in Immunology…
Drew Weissman identified his interest in basic scientific research — the beginning research stages that lay a foundation for future applications — early in his academic career. By the time he received his MD PhD in Immunology and Microbiology from Boston University, he had focused in on dendritic cells, which recognize foreign bacteria and viruses, then initiate immune reactions to fight off the invaders.
In 1990, Weissman began a fellowship at the National Institutes of Health (NIH), where he worked in Dr. Anthony Fauci’s lab. Fauci was not yet a household name but did carry weight in the field, as he was the director of the National Institute of Allergy and Infectious Diseases (NIAID), where he led a lab that studied the immunology of HIV. Weissman developed his own section within Fauci’s lab where he had a wide reign to pursue various research interests, other than vaccine research, which wasn’t performed in the lab.
“Of course,” Weissman says, “That meant when I got my own lab at the University of Pennsylvania, I wanted to study vaccines.” That decision primed him for precisely the basic research that would translate to a massive impact on the COVID-19 pandemic.
Chocolate and Peanut Butter
When Karikó and Weissman teamed up, both researchers remember the work itself as what kept them collaborating. “It was stimulating,” says Karikó, and that was important because in the beginning, it was just Weissman and her in the lab. Karikó remembers reading papers at 3 a.m. and receiving an email from Drew, who was also awake. She felt solidarity with her research partner, both sleep-deprived but determined to press on.
By its nature, Karikó and Weissman’s research was cross-disciplinary. Karikó’s specialty in the molecular biology of RNA complemented Weissman’s expertise in vaccinology and immunology. Karikó produced the RNA while Weissman grew and worked with the cells. They inserted mRNA into dendritic cells and found that the dendritic cells were incredibly good at taking in mRNA, reading it, and producing protein based on the mRNA code. But when they tried to translate the technique to live mice, it didn’t work. The mice got sick; they looked lethargic and stopped eating.
But Karikó and Weissman saw progress in each experiment. “We were getting interesting results, so they just kept leading us on," Weissman says. Though it was tough to find funding — private investors also showed a lack of interest — Drew had grants to support his lab, and they were able to scrape together funding (largely from NIH) to continue their research.
Weissman’s experience in immunology led them to an explanation for the mice’s poor reaction — a phenomenon previously only thought to be caused by DNA. Research had shown that when foreign DNA is introduced into the body, the immune system flags it as an intruder and triggers a serious inflammatory response. The first time Weissman added mRNA to dendritic cells, he saw an incredible level of inflammation, and his experiments showed that mRNA triggered the same immunogenic effect in mice, causing a dangerous inflammatory reaction.
Along with the excitement at figuring out the reason for the roadblock, Karikó recalls a sense of dread. She had dedicated a decade to developing mRNA with the hope of creating a therapy, the whole time unaware that the mRNA she produced had dangerous effects. Was it all for nothing?
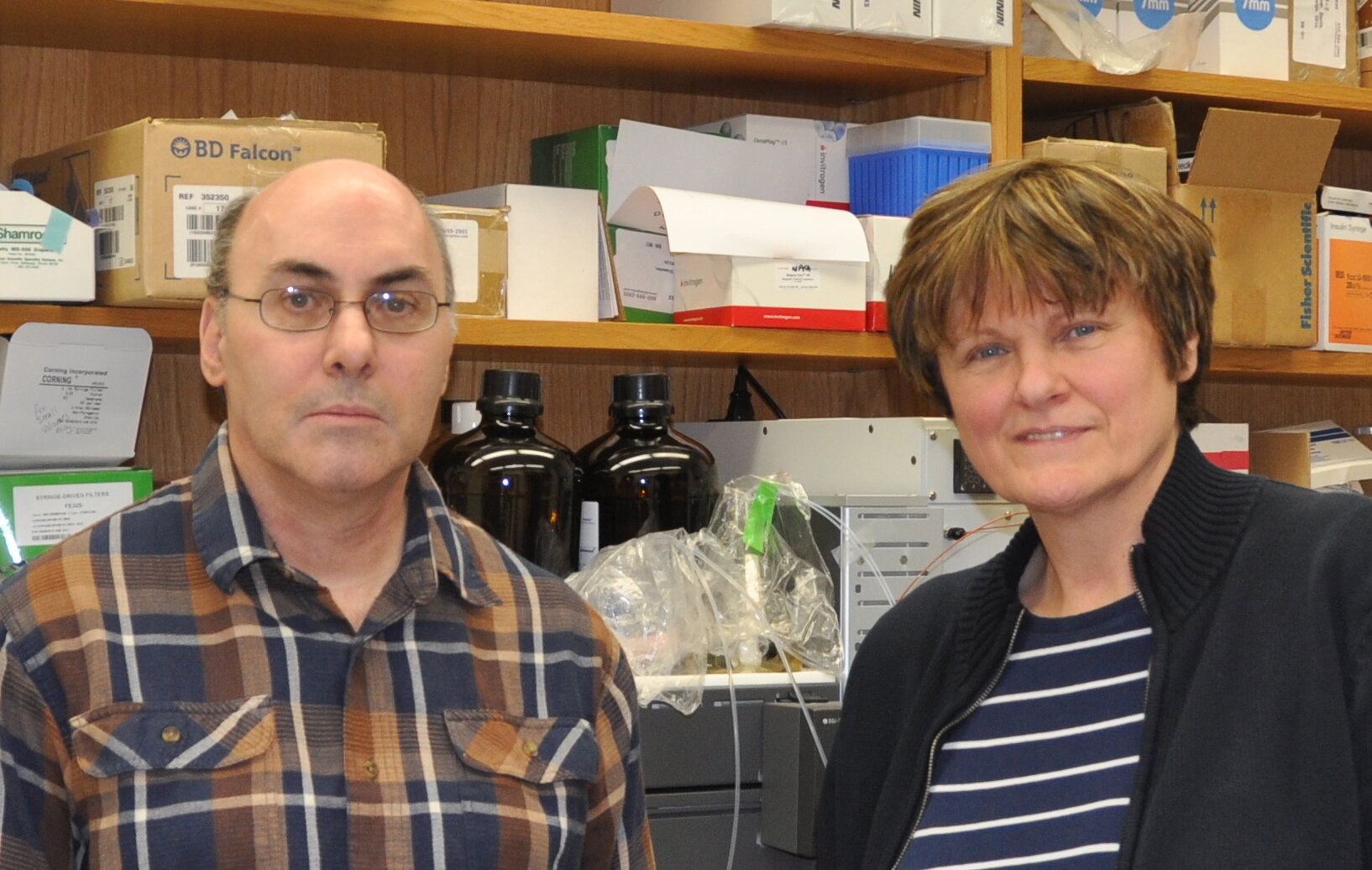
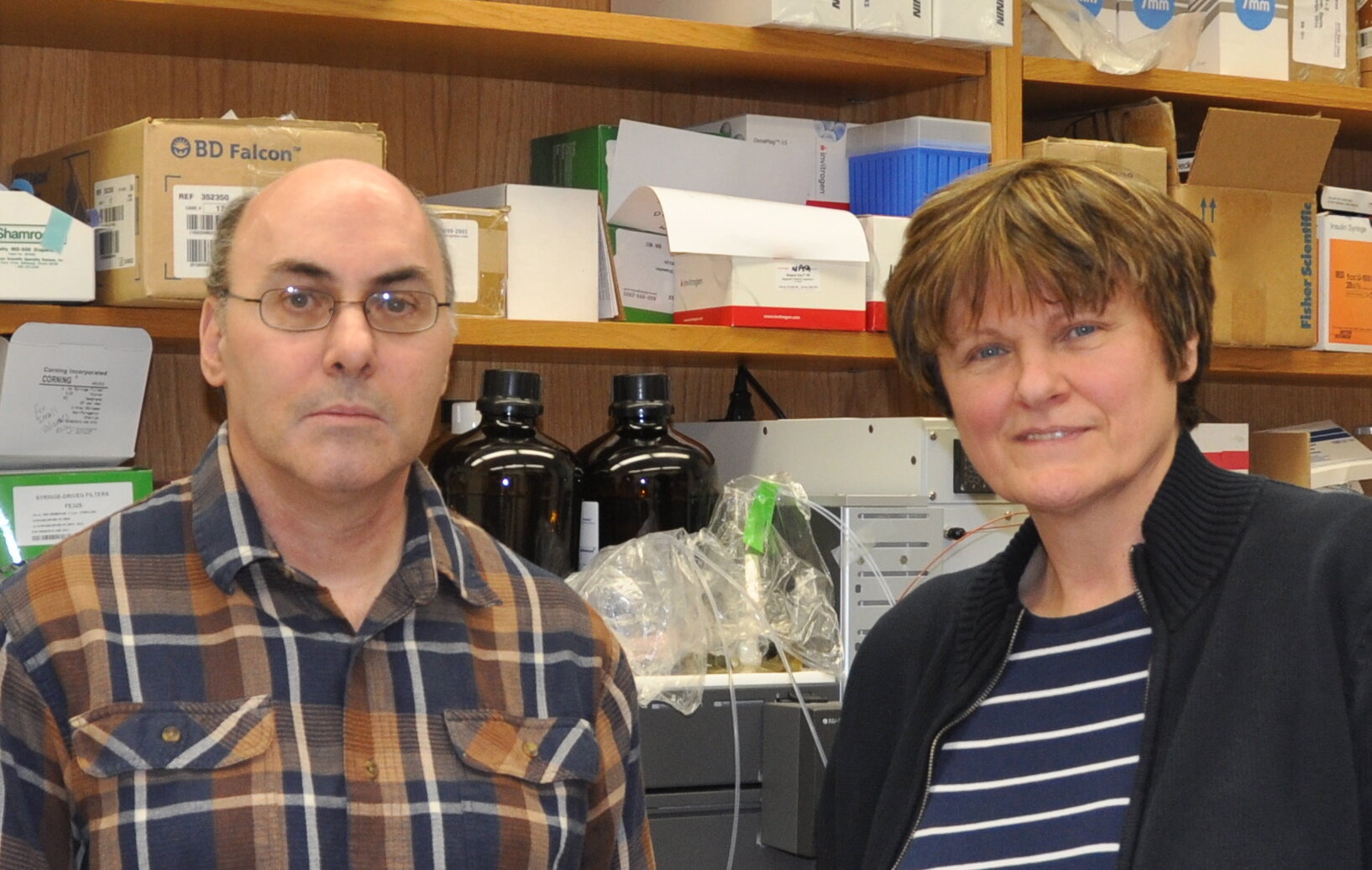
Weissman and Karikó in 2015
The Ol’ Switcheroo
Karikó’s experience synthesizing mRNA enabled her to make structural changes to the molecule, so she and Weissman wondered if they could alter the mRNA just enough that the immune system wouldn’t recognize it as an intruder. They zeroed in on nucleosides, the building blocks of RNA, which, coincidentally, Karikó had worked on during her PhD research. They also found that another form of RNA, transfer RNA (tRNA), did not cause an immune reaction like synthesized mRNA does. By subbing tRNA modified nucleosides for mRNA nucleosides (one at a time), they could potentially identify the source of mRNA’s dangerous immune response.
First, Karikó had to acquire the molecules, which presented some limitations. These molecules aren’t available at the local grocery store; scientists acquire materials from chemical supply companies, and Karikó found that only ten different types were available to order. She got all of them, crossed her fingers, and hoped that one would be right. Of the ten Karikó tested, only three were viable, leaving her with low odds that one of them would be the key to circumventing the mRNA immune response.
Astoundingly, one of the three did exactly that: a molecule found in tRNA called pseudouridine, which is a slightly modified version of the mRNA molecule uridine. When Karikó tested the mRNA with pseudouridine, the immune system’s alarm bells were silent. And not only that — inserting the mRNA into cells translated to a tremendous amount of protein production. That one change opened the door to a huge number of therapeutic applications. Karikó and Weissman’s long hours and late nights had paid off.
In a reversal of his usual role as the skeptical and grounded half of the duo, Weissman was sure the discovery would be a big deal, and invitations to give scientific talks would soon pour in. But when he and Karikó published their findings in 2005, it barely registered as a blip on the scientific community’s radar. They later found out that an editor of the scientific journal had even needed to advocate for the paper to be published because other editors did not see the merit of the discovery.
Yet Karikó and Weissman knew the potential. They patented the modified nucleosides and even started their own small biotech company, RNARx. In 2012, Karikó and Weissman showed that their modified mRNA was not only safe to inject in animal models, but it could make them healthier than before. Translation to humans seemed possible, particularly as a platform for vaccines. Due to its quick disintigration, mRNA has the potential to compel cells to produce a preview of a virus without sticking around long enough to disrupt cellular processes.
The scientific community began to recognize mRNA’s merit as research on a Zika vaccine showed promise, and later, applications of mRNA vaccines against other pathogens like the influenza virus and HIV were successful in animal models. However, funding for vaccine research is tough to generate because monetary return on investment is usually small, so it was slow going. In 2020, however, everything changed.
RNA Responders
Suddenly, funding for vaccines was abundant as the world scrambled to combat the 2020 COVID-19 pandemic. Research was fast-tracked. Weissman’s lab began working on a vaccine the day the virus’ genetic sequence was released. Evidence of mRNA-based vaccines’ effectiveness began to emerge, and though exciting, the results were not surprising to Karikó and Weissman.
The validation was a long time in coming. Each celebrated in their own way — Karikó with Goobers chocolate-covered peanuts and Weissman with takeout from an Italian restaurant. In December 2020, two mRNA vaccines — made by a Pfizer-BioNTech partnership and Moderna — were the first SARS-CoV-2 vaccines to receive emergency use authorization from the U.S. Food and Drug Administration (FDA), the fastest vaccines to ever be developed.
Karikó and Weissman are quick to emphasize that their research is built on a foundation of the work of scientists before them. mRNA was discovered in 1961, and the invention of the PCR technique in the 1980s, which generates millions of copies of DNA or RNA from a tiny sample, allowed Karikó to synthesize cleaner, better RNA a decade later.
The NIH grants that funded Karikó and Weissman’s research were also essential to the development of mRNA therapeutics. However, it is important to acknowledge the magnitude of strain that the initial lack of funding placed on the researchers. While Karikó and Weissman’s determination and clearsightedness unlocked the potential held by mRNA, their struggle to obtain funding is emblematic of countless researchers who hold the promise to make lifesaving discoveries but find themselves without the resources to do so. Robust federal funding can help deliver on that promise.
Today, Karikó and Weissman are not resting on their laurels. Weissman’s lab at Penn is already looking toward the next pandemic, investigating a pan-coronavirus vaccine that will protect against coronaviruses that appear in the future and developing a gene therapy that will allow widespread treatment for a variety of diseases. Karikó, currently overseeing mRNA work at BioNTech, also sees applications of mRNA technology in treatment for many diseases, including multiple sclerosis and sickle cell disease. Back in their conversations by the photocopier, neither could have foreseen the magnitude of payoff their work would generate. Now, in the second year of the COVID-19 pandemic, and in the midst of a surge of mRNA therapeutics research, it is clear that this technology — which has already saved millions of lives — will save many more lives in the years to come.
By Gwendolyn Bogard